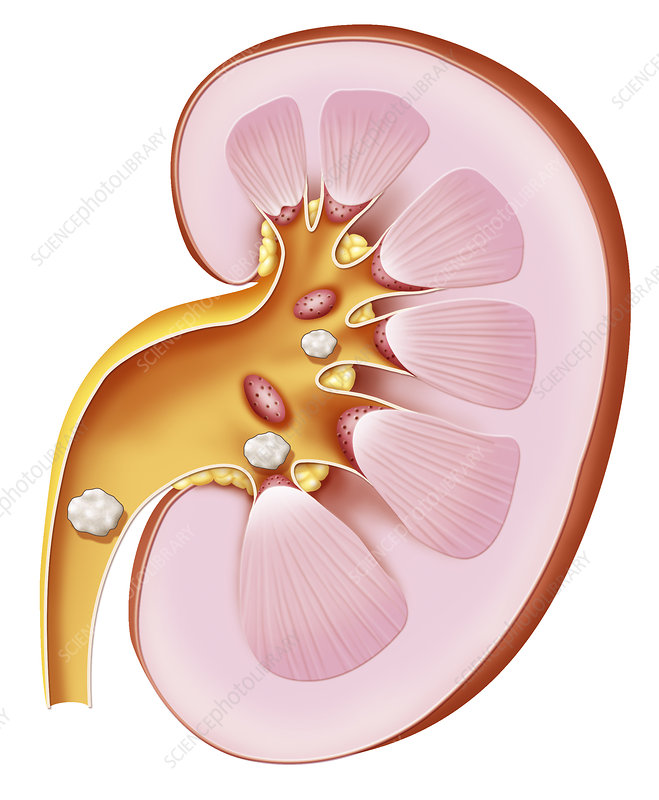
Kidney stones come in a variety of forms. They’re caused by the precipitation of something – either because their quantity is large or due to decreased intravascular volume. Each type has its own risk factor, which is why there needs to be a close analysis of both the stone and the urine after the stone passes.
EtiologyThe typical patient will present with colicky flank pain that radiates to the groin and with nausea / vomiting. This presentation may mimic pyelonephritis (look for a fever and white cell casts) and renal cell carcinoma (look for a palpable mass).
Because of the similarities between diseases, start with a urinalysis. The absence of casts and the presence of blood (even microscopic hematuria counts) is indicative of the stone. In the absence of microscopic hematuria, the likelihood of a symptomatic stone is quite low.
InvestigationsThe diagnosis is confirmed with a Non-contrasted CT scan – by far the best test. There will be times where that test is not available, as in pregnancy. If pregnant, use ultrasound. While ultrasound may not be as sensitive for distal stones or hydroureter as CT, it can be done safely without exposing the fetus to radiation. KUB should NOT be used for diagnosis, but can be used to track disease progression in known stone disease.
Management
Management is based on the size of the stone:
If <5 mm the stone will pass spontaneously. Hydration and pain control is all that’s needed.
|
If <7 mm use medical expulsive therapy. This is achieved with Calcium Channel Blockers (Amlodipine), Alpha-Blockers (Terazosin) or both.
If <1.5 cm, the stone is unlikely to pass on its own and needs to be broken down. Both ureteroscopy (for distal stones) and lithotripsy (for proximal stones) are appropriate.
If >1.5 cm, the stone will need to be resected. This is done either with laparoscopic exploration (proximal stones) or with percutaneous anterograde nephrolithotomy (distal stones).
If emergent, decompression of the GU system is required. As in the case of obstructive sepsis, either a stent (distal disease) or nephrostomy (proximal disease) is indicated.
Regardless of the way the stone’s taken out, it needs to be analyzed. See the chart on the top of the page for composition of different stones. Then, 6 weeks later analyze a 24-hr urine. Correct the risk factors and bam! good as new.
