Definition
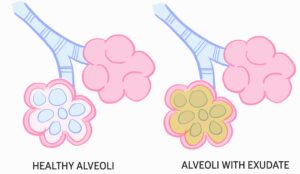
Pneumonia is a lower respiratory tract infection characterised by inflammation of interstitial tissue and/or alveolar space of lungs.
Categories according to timing:
- Community Acquired Pneumonia (CAP)
- Pneumonia in a patient in the community or hospitalised for less than 48 hours
- Hospital Acquired Pneumonia (HAP)
- Pneumonia that develops in a patient who has been hospitalised for more than 48 hours
- Ventilator Associate Pneumonia
- Pneumonia that develops in a patient who has been intubated for more than 48 hours
- Aspiration Pneumonia
- Pneumonia developed after contents from the stomach or mouth enters the lungs
- Abscess likely and foul-smelling sputum
Categories according to anatomy:
- Lobar Pneumonia
- Pneumonia localised to one pulmonary lobe
- Bronchopneumonia
- Pneumonia localised to bronchioles and adjacent alveoli
- Interstitial Pneumonia
- Pneumonia causing fibrosis of interstitial tissue
- Cryptogenic Organising Pneumonia (COP)
- Inflammatory tissue present in bronchioles and alveoli
- Although classified as pneumonia, it is non-infectious
- Only diagnosed when other causes of pneumonia are eliminated
Categories according to clinical presentation:
- Typical
- Productive cough present
- Common pathogens:
- Streptococcus pneumoniae (most common lobar pneumonia)
- Moraxella catarrhalis, Hemophilus influenzae (COPD exacerbations)
- Staphylococcus aureus (IV drug users)
- Klebsiella pneumoniae (alcoholics, aspiration pneumoniae, diabetics, malnourished)
- Atypical
- Dry cough
- Auscultation unremarkable
- Common pathogens:
- Mycoplasma pneumoniae
- Chlamydophila pneumoniae
- Legionella pneumophila
- Impaired mucociliary escalator causing stasis/accumulation of secretions (smoking, CF, bronchiectasis)
- Immunocompromised (Pneumocystis jirovecii, Aspergillus fumigatus, candida species, CMV)
- Poor cough/gag reflex or increased risk of aspiration (stroke, GORD, low GCS)
- Obstruction like space-occupying lesions
- Cough ± sputum
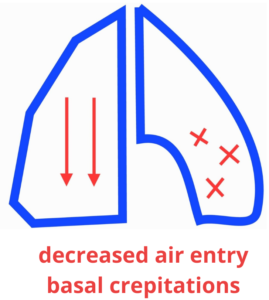
- Shortness of breath
- Fever/ chills/ rigors
- Pleuritic chest pain
- Papular rash
- Diarrhoea
- Neurological changes
- Vitals signs
- Glasgow Coma Scale (GCS): to assess neurological changes
- FBE: elevated neutrophil count
- CRP: elevated
- UEC: presence of uraemia demonstrates high severity
- Sputum MCS and blood culture if febrile
- ABG and PCR if suspecting viral illness
- CXR for new/persistent infiltrate
- O2, IV fluids and salbutamol if necessary
- Antibiotics:
| Low severity | Moderate severity | High severity | |
| CAP | Amoxicillin if typical; Doxycycline OR Clarithromycin if atypical | Benzylpenicillin PLUS Doxycycline OR Clarithromycin | Ceftriaxone |
| HAP | Amoxicillin PLUS Clavulanate | Amoxicillin PLUS Clavulanate | Piperacillin PLUS Tazobactam OR Cefepime |
